|
Workflow and 8 pitfalls that can impair a practice's efficiency
(And how a distributed teleradiology reading platform can transform your practice)
Dr. Casey is the CEO and Co-Founder of Virtual Radiologic Corporation, Minnetonka, MN.While most radiologists today have made the transition from film-based analog interpretations to digital interpretations using a picture archiving communication system (PACS), most of us are still remarkably far from reaping the potential efficiency benefits of this digital transition. Some may even find themselves in a less efficient practice environment than in the “good old days” of film-based reads. Back in those days, analog reading workflows had evolved to maximum efficiencies over a period of several decades. While great technology advances have been made over the past decade with the widespread introduction of PACS, radiology information systems (RIS), and voice recognition, there has, unfortunately, been much less thought put into developing efficient digital workflows. Many of us actually faced a setback in efficiency when we transitioned to the use of PACS and/or voice recognition. Case volumes are growing yearly because of the aging population and the advancement of imaging technologies. Declining per-study reimbursements require efŮciency gains to make up the per-unit losses with higher volume. In order for a practice to succeed in recruitment and retention, salaries must be competitive. If the workflow is not efficient, a practice will have trouble maintaining market-competitive radiologist salaries .
Workflow is driven by worklists
In order to address deŮciencies, it is important to analyze what is driving the work▀ow in a given practice. Typically, this is obvious from the main worklist used by the practice to choose the next case. Practices generally fall into several categories of work▀ow:
Each of these workflows has its loyal supporters. The problem with these conventional workflows is that they are typically driven by “dumb” worklists. These are retrospectively and passively sorted lists that are prioritized by time, modality, location, or a combination of these factors. The main problem with these worklists is that they do not offer real-time feedback and, as such, concepts such as active load balancing of studies and prioritization of cases according to specific turnaround time (TAT) needs are not considered. Because of these inflexibilities and a lack of systems integration, many practices actually continue to work from paper lists. Paper-based workflowDespite having successfully made the transition from analog film-based reading to digital PACS-based reading, many practices persist in using stacks of papers as their worklists. These are typically control sheets printed from the RIS. For teleradiology practices, these are typically stacks of inbound fax orders. The appeal of the paper worklist is that it can be shuffled in a much more flexible fashion than most dumb digital worklists. Emergency cases can easily be pulled right to the top of the stack. Furthermore, a barcode on the sheet can overcome the lack of system integration: it serves as an analog-to-digital interface between the PACS, RIS, and dictation system. Problems occur when the stack of papers is too large to divide among a sizable practice across multiple facilities. Furthermore, sheets are prone to being lost, and the TAT on the case could be severely delayed. Custom workflow driven by a workflow engine software A new type of customizable worklist is the workflow engine. This takes into account the unique requirements of a practice, including multiple-case TAT requirements, various subspecialty assignments, and the overall size of the group. This software can be built into the PACS, the RIS, or the dictation system but can also exist as an independent software application. One can think of it as yet another work-list, but it is an active real-time worklist that is focused only on workflow. It drives case assignments on the basis of many factors such as license, credentials, subspecialty, TAT requirements of the case, and load balancing of workloads across radiologists in the practice. Assignment by license and credential is particularly critical to a multistate teleradiology practice as a protection against radiologists doing unauthorized interpretations. Each radiologist can actually have an individual worklist, which, on a Web-based system, will be available wherever he or she chooses to read. As compared with a passive worklist that changes only as new patients are added or as existing cases are read, an active worklist on a workflow engine can dynamically rearrange the assignments of cases to a given radiologist; eg, an emergency brain MRI will go to the top of the neuroradiologist’s worklist even if older, but less critical, cases are present.
Eight imaging workflow pitfalls
Regardless of which type of worklist your practice uses, you will improve your workflows by avoiding as many of the following pitfalls to efficient workflow as possible.1. The “dumb” worklist The use of a dumb worklist results in frequent interruptions and radiologist cherry-picking. The nonprioritization of cases by TAT on a nonintelligent worklist or the loss of cases (due to accidental sign-off on a digital worklist or a lost sheet on a paper worklist) results in a greater chance of an interruption, such as a clinician inquiry. Furthermore, the simplest of the dumb worklists (such as used on a PACS) allows for radiologists to arbitrarily choose whichever cases they will read. Nearly all currently used worklists allow radiologists to jump ahead to grab cases out of order. When this is done for self-serving reasons, such as to skip a difficult case or to grab an easy case, it is called cherry-picking. The downsides of cherry-picking are obvious: this is antiteam behavior that dumps work on one’s colleagues, and it hurts patient care by delaying the TAT on complex cases. While some cherry-picking probably exists to various degrees in any mid-size to large practice, distributed practices are even more prone to this workflow vice, as it cannot be policed merely by a disapproving stare from across the reading room. Furthermore, a dumb worklist may assign cases to a single radiologist in a single location, and then case turnaround performance will be dependent on that radiologist’s availability. If the chosen radiologist is busy doing a procedure or is on a lunch break, the TAT on the case will be delayed. Load balancing across radiologists and locations accesses a larger pool of potential readers and eliminates dependence on the availability of a single radiologist. Many radiologists perform teleradiology with case assignments on older-architecture point-to-point digital imaging and communications in medicine (DICOM) teleradiology systems, and this limits the ability to load balance studies across multiple radiologists and multiple locations. More modern Web server architectures tend to better support such load balancing, as they permit simultaneous downloads to multiple locations and radiologists. The best way to avoid the pitfall of the dumb worklist is to switch to a workflow driven by an intelligent worklist, which will minimize interruptions and cherry-picking and will allow load balancing to provide the greatest consistency of TAT performance. 2. Vision-dependent workflow navigationThis is a very common pitfall. It is perhaps often overlooked because it costs only a second here and a second there. But if you add up the seconds over the entire work day, and it amounts to real time and resistance to stress-free workflow. This should be a very simple concept: since image interpretation can be condensed down to the radiologist looking at images, anything that requires the radiologist to remove his or her eyes from the PACS images is potentially unnecessary and thus a potential impairment to workflow efficiency. The common culprits that require the radiologist to remove his or her focus from the PACS images are: worklists, computer menus, toolbar icons, keyboards, and dictation screens. Ideally, a radiologist should use as much “eyes-free” navigation of the reading platform as possible. If possible, right-click mouse menus and toolbars should be avoided in favor of keyboard shortcuts, especially if they can be mapped to supplementary mouse buttons or some other human interface device (such as a dictation microphone, grip, jog dial, or foot pedals). Nearly every common PACS function should be able to be navigated while dictating, without having to stop scrolling or to take one’s eyes off the images. Furthermore, it is ideal to minimize the time spent looking at the voice-recognition screen. 3. Comparison cases on film or diskOne of the most frustrating experiences in workflow is having to compare a case on your current PACS with the patient’s relevant prior examination on film, on an older PACS system, or on an outside CD/DVD. This entails mental and physical strain, since the light-box or accessory viewing monitor is often not within easy reach. Furthermore, the controls on the viewer from the external CD/DVD are likely unfamiliar and frustrating to use. To avoid this pitfall, the films or old PACS data can be imported into the new PACS system, but this is certainly an added cost. One can consider building an old case archive within the new PACS over a period of time before going live with the new system. Ideally, external CD/DVD data should be able to be imported into the PACS system. This is particularly important in a distributed practice, in which it helps to avoid shipping films and disks between reading sites. Unfortunately, some systems are not flexible enough to allow this without risking data corruptions, and, furthermore, some of the CD/DVD cases are not in an importable DICOMDIR format. 4. Working from multiple worklists on multiple computersAlthough every practice has to choose a primary worklist from which to drive its workflow, many practices persist in the use of multiple worklists because of the lack of integration among applications. Ideally, the primary worklist is all that is needed. It should launch the PACS images and open the RIS study information and the dictation window. The use of ≥2 computers creates user confusion, as the radiologist typically needs to shift back and forth between multiple keyboards and multiple mice. To get past this mess, a practice needs to achieve not only desktop-level integration but also application-level integration. Desktop-level integration—Desktop-level integration gets all of a radiologist’s work applications onto a single computer (although it can still have multiple viewing monitors). Application-level integration—Application-level integration is an even higher level of integration that gets the individual software applications (such as the PACS, the RIS, and the dictation system) to behave as a single functional unit on 1 computer. This level of integration results in a single worklist that launches all of the software components needed for case viewing and dictation. There is no need to select patients from separate worklists, and this eliminates the risk of human error in selecting a wrong patient match on the secondary worklist. Integration of PACS, RIS, and dictation systems is one of the biggest safety improvements that informatics can contribute to radiology. Such levels of integration are perhaps easier said than done. Unfortunately, PACS–RIS integration may require cooperation between competing software vendors. More modern Web-based PACS systems tend to make integration easier by means of URL integration: the PACS images can be launched by any worklist that is able to predict the Web address of the images from the known patient demographics. 5. Inadequate bandwidth, network bottlenecks, and/or poor cachingMany hospitals have an inadequate hosting environment or suboptimal connections to the Internet. Applications hosted on servers from within the hospital or within its data center might work fine within the hospital local-area network (LAN) but often are suboptimal for use over a wide-area network (WAN) such as the Internet. Many hospitals have low-capacity encryption devices (virtual private networks [VPNs] or Secure Sockets Layer [SSL] accelerators), which essentially place a cap on the available bandwidth to those outside the firewall. Do not skimp on information technology (IT) hardware and bandwidth. You will pay the price in radiologist efficiency. It is amazing how tolerant radiologists can be when using teleradiology systems. On the old telephone-based teleradiology systems, radiologists became accustomed to waiting for cases to download. In the modern era, it should be unacceptable for a radiologist to have to wait for data to transmit after a case is launched. All data transfers should occur before the case is viewed. Such predelivery of data is termed caching or precaching. Certainly, even over high-speed Internet connections, cases take time to transmit, especially in the era of large multidetector CT studies. If a workflow engine can predict the cases that are the next most likely to be viewed, however, then all of the transfer time can occur in the background while the radiologist is reading the current case. On a well-designed system, the radiologist should perceive no performance degradation or delay between cases when using a PACS onsite on the LAN versus using the same PACS as a teleradiology system over the Internet. On a poorly designed system, one can wait seconds to minutes between cases for data to download. If this takes 2 minutes on average per case, over a 120-case workload, this will add up to 4 hours of wasted time! Poor bandwidth or poor caching impairs efficiency and can destroy the economics of a distributed practice. 6. Multiple disparate PACS, RIS, and dictation systems in multiple locationsThis problem plagues mid-size to large groups with multiple locations. Often, the locations are not part of the same healthcare system and do not use the same brand of software applications. As such, these groups work from multiple different workflows, which is inherently inefficient. Each system comes with a different workflow along with a different username and password (and these change at all too frequent intervals). Each different brand of system has its own unique software user interface. Not all PACS even use the same keyboard shortcuts or navigational controls. As such, when rotating to a new facility, radiologists spend some time working at a lower efficiency because they are not familiar with the system. In a distributed practice, it is challenging to work on multiple different systems. This can result in radiologists working in a “war room”–like environment that is filled with computers among which they need to rotate to do their reads. At best, these practices use a paper worklist composed of faxes. At worst, they don’t have a real master worklist between applications and instead work on individual disjointed worklists. The conventional alternative is even worse: driving between facilities or working in isolation from the rest of the group in a single facility. This results in wasteful travel time, poor ability to balance workloads, and poor degrees of subspecialization and intrapractice consultations, even for large groups. Such a heterogeneous set of workflows is not scalable as a practice grows. If your group wishes to grow and to improve efficiency, it is critical to minimize the number of different systems from which you read. While it might not be possible to remove the multiple systems on which the affiliated hospitals depend, it is possible to aggregate one’s work (or at least one’s interfacility load-balancing work) across your facilities onto a single reading platform. Such a reading platform can be the one and only reading platform for a practice that overlies all of the heterogeneous facility systems. In this way, a distributed practice can use a single worklist to drive a unified workflow. 7. Physicians performing nonphysician workTo improve workflow, it is critical that doctors not perform nonphysician work. In any organization, the staff member who is paid the most should be limited to doing what only he or she can do. Radiologists are more expensive than phone operators; therefore, radiologists should not be working the phones. They should indeed be available for phone consultation but should not be trying to track the whereabouts or phone numbers of the ordering or on-call clinician. Most radiologists can interpret a head CT faster than they can manually fax its report! Radiologists are more expensive than automated fax servers and should not waste time operating fax machines. One of the most common causes of malpractice suits involves the miscommunication of results—particularly the failure to notify clinicians of important findings. In a typical practice, a radiologist might waste precious time trying to track down a clinician. Such nonphysician work can be an obstacle course that frustrates and distracts the radiologist. After multiple attempts, a radiologist might forget about the notification task altogether. This can inadvertently lead to serious patient care issues. In my practice, we have set up a call center whose staff does the behind-the-scenes, nonphysician work of tracking down clinicians and technologists. Furthermore, we have built its functionality into our workflow engine/reporting software. Once a radiologist sees a critical finding on an image, a single mouse-click can trigger a critical-finding call request to our call center. The exact time of the request is stored in our software as an audit trail. As soon as the clinician is located and on the phone line, the radiologist is connected to the phone call. Removing this nonphysician receptionist activity allows a radiologist to stay focused on what he or she does best: reading images. This type of system can be a major efficiency gain for almost every practice. 8. Outdated, nonupdatable systemsThis problem is created by legacy systems that required substantial up-front capital to install but then remain relatively stagnant throughout their life cycle. A hospital will seek a return on investment (ROI) on the software and likely will not have planned for major software upgrades in its tight annual budget. As a result, a practice may be stuck with outdated software for years even if the larger multidetector data sets are already bringing it to its knees. This is perhaps the most serious workflow problem, since it limits a practice’s ability to maintain state-of-the-art technology. Unless it is possible to customize or integrate the existing applications, a practice is relatively powerless to improve its workflows.
Improvements to efficiency via a distributed reading platform
One way to escape most, if not all, of these workflow traps, is to consider investing in an overlying distributed reading platform. Fortunately, such Web-based systems are more affordable than the legacy systems with their old school “big iron” workstations. Application Service Provider (ASP) and Software as a Service (SaaS) offerings allow you to avoid large upfront capital purchases and are typically available for a subscription or per-case fee. These systems are usually hosted by the software provider, which saves significant data center and IT personnel costs. Instead, these costs are shared across the customer base, and your share is charged to you within the subscription fee. Such software is integrated, deployed, and frequently updated over the Internet such that it is always state of the art. It runs on inexpensive PC hardware.
Load balancing in a distributed practice
A distributed reading platform can provide an intelligent worklist, which will be able to determine the ideal reader for a given case at any moment in time. Such an intelligent worklist assigns cases to radiologists on the basis of the radiologist’s credentials, subspecialty, and current workload. This case assignment feature serves to load balance studies across multiple radiologists and facilities. For example, if all other factors are equal, a simple case assignment algorithm will give a new case to the radiologist with the shortest worklist. This tends to prevent situations in which one radiologist is bogged down with a large worklist while another may have an empty list with no work to perform. A larger distributed practice can better take advantage of load balancing across its reading locations while also leveraging overlapping shifts to maintain the greatest consistency of TATs. In a non-distributed smaller practice, there is no load balancing across facilities, and thus there is limited ability to leverage overlapping shifts. The level staffing of such a facility during a shift results in TATs that are relatively proportional to the hourly case volume at any given hour. The smaller the practice, the more the case TAT is held hostage to the health, availability, and mood of a single radiologist. In larger practices, variances in daily performance or the availability of radiologists will tend to be masked by the overall pool of radiologist capacity. In my own practice, we have made great improvements in the consistency of our TAT by leveraging the entire size of the distributed practice with load balancing and overlapping shifts (Figures 1 and 2). |
|
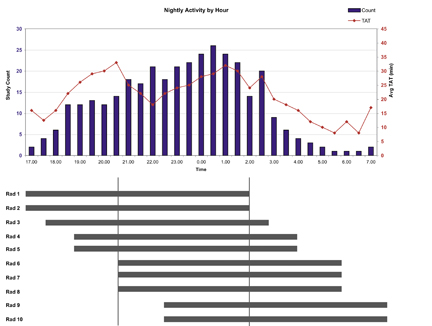
FIGURE 1. Inconsistency of turnaround times (TATs) in a small teleradiology practice with flat staffing. This graph represents an approximation of the typical nightly performance in Virtual Radiologic 6 years ago when the practice was substantially smaller. While average study TATs were acceptable at approximately 20 minutes, there was significant variability in TAT performance, with deterioration in the evening (just prior to a 9 pm shift change) and just after midnight (during peak nightly volume). The flat staffing of 2 radiologists during the night had to contend with fluctuations in case volume. This spilled over into inconsistency of TAT performance. Depending on the time during the night, the radiologists either had too few or too many cases to read.
|
|
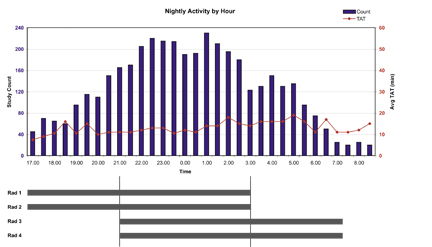
FIGURE 2. Stable turnaround times (TATs) in a large teleradiology practice with staggered staffing. This graph represents the performance of our practice (Virtual Radiologic Corporation, Minnetonka, MN) on a recent night and depicts the power of load balancing and staggered shifts in a distributed large practice. Because the hourly staffing levels have been set to match the case volume distribution, there is a consistent level of staffing throughout the night and resultant consistency of TATs. A large distributed practice allows for better forecasting of hourly case volumes and corresponding staffing needs (demand versus capacity). This has lowered TATs to an average of 13 minutes, with minimal variability during the night. The radiologists have appropriate individual workloads throughout the night, despite predictable fluctuations in practice case volumes during the night.
|
|
Conclusion
Because attention has not been paid to workflow, the expected efficiency gains of the digital era have not yet been fully delivered to radiologists. Analyzing a practice’s workflow and avoiding a host of workflow pitfalls can provide significant improvements in efficiency. Most of the solutions to the pitfalls require investment in upgraded or new systems, custom integrations, or IT infrastructure. Given that the legacy systems that force the workflow pitfalls upon radiologists are provided by facilities to radiology groups for “free,” there is an expected reluctance to invest in an IT infrastructure or a common reading platform for a practice. What is often overlooked is that there is a cost to the “free” legacy software that is paid dearly with decreased radiologist productivity. Major efficiency gains among your practice’s radiologists can not only pay for the new distributed workflow technologies but can also be your best way to defend against the never-ending trend of declining reimbursements. |